
Matula Thoughts February 7, 2014
Michigan Urology Family
Curiosity, novelty, and the elements of change: Norse mythology, ICD-10, PACs, and other thoughts.
 Today, February 7th is the 38th day of 2014 and given our recent experience with the arctic temperature blasts and deeper snow than we’ve seen in Ann Arbor in many years, who cannot yearn for those lovely Michigan summers? (Picture from “Up North” in summer with 4-legged Molly seeking a dietary novelty, held barely out of range by Charlotte) By the way, in case you are curious, 2014 is NOT a leap year, so we have only 21 more days of February and 327 days in this calendar year to extend our curiosity and good work in the Department of Urology at the University of Michigan. So you might ask, is the glass partly empty or mostly full? While a matter of one’s perspective, the latter viewpoint is the more productive option, as it conditions us to seek comfort and novelty in that glass of opportunity. All of us crave novelty just as do Charlotte and Molly. Novelty rewards curiosity, a driving force for most living things. We enjoy novelty in the arts and our department celebrates this yearly during the Ann Arbor Art Fairs in July with the Chang Lecture on Art and Medicine. This will be our 8th year for it and our speaker will be James Ravin, an ophthalmologist at the University of Toledo. He was educated and trained here at Michigan and is co-author of a wonderful book The Artist’s Eyes. As you look forward to the summer, consider coming to the Art Fairs and stepping out of the heat late on Thursday afternoon (July 17, 5:00 PM, University of Michigan Hospital, Ford Auditorium) to hear Dr. Ravin.
Today, February 7th is the 38th day of 2014 and given our recent experience with the arctic temperature blasts and deeper snow than we’ve seen in Ann Arbor in many years, who cannot yearn for those lovely Michigan summers? (Picture from “Up North” in summer with 4-legged Molly seeking a dietary novelty, held barely out of range by Charlotte) By the way, in case you are curious, 2014 is NOT a leap year, so we have only 21 more days of February and 327 days in this calendar year to extend our curiosity and good work in the Department of Urology at the University of Michigan. So you might ask, is the glass partly empty or mostly full? While a matter of one’s perspective, the latter viewpoint is the more productive option, as it conditions us to seek comfort and novelty in that glass of opportunity. All of us crave novelty just as do Charlotte and Molly. Novelty rewards curiosity, a driving force for most living things. We enjoy novelty in the arts and our department celebrates this yearly during the Ann Arbor Art Fairs in July with the Chang Lecture on Art and Medicine. This will be our 8th year for it and our speaker will be James Ravin, an ophthalmologist at the University of Toledo. He was educated and trained here at Michigan and is co-author of a wonderful book The Artist’s Eyes. As you look forward to the summer, consider coming to the Art Fairs and stepping out of the heat late on Thursday afternoon (July 17, 5:00 PM, University of Michigan Hospital, Ford Auditorium) to hear Dr. Ravin.- Curiosity drives discovery, a fundamental expectation of society for enterprises such as our university, our medical school, and our Department of Urology. We have been pretty good at discovery for a century of urologic practice, education, and research in Ann Arbor. Intellectual curiosity gets expensive, but it must be supported. A hundred years ago our curiosity was funded by the faculty themselves and the hospital. That is, some dollars from the practice of health care were turned to the academic mission of educating the next generation and discovery of new knowledge. After WWII, the federal government recognized the essential national priorities of education and research, thus federal funding came to dominate health care research. Massive structures were necessary to play in that important game of discovery. (Just look in our back yard at Med Sci I & II, the VA research buildings, Med Sci Research Buildings I-III, The Life Sciences Institute, BRSB, North Campus).
- Deliberate contraction of that national agenda and foolish sequestering have downshifted that funding, transferring more cost of maintenance of the physical and intellectual infrastructure to medical schools. This makes the picture bleak for today’s budgets, and bleaker for tomorrow’s discovery. The frost is lifting a little, perhaps as you look at Congress’s funding projections, but we are sadly below where we should be in terms of nations R & D. The paradox is that on one hand as we assign blame for the downshifting of research funding to the “limited resources” of our national wealth, we seem oblivious to the fact the wealth of nations and the health of nations derive from discovery. Thor’s hammer of sensibility will not be coming down on Washington anytime soon, so we need to live with this new normal and create a new paradigm of medical education and research, or rapidly shutter expensive buildings and repurpose talented researchers.
- Politics and politicians that set the national agenda and policies are important to our self-interest. Courts have recently decided that influence from political action committees (PACs) should not only be protected, but even expanded. Therefore you and I cannot remain mere witnesses to the political game. We need to be open-minded to different ideas, but find and support niches that resonate with our interests. The AUA and ACS PACs represent our profession reasonably well and need our support. They are part of political life today and we can’t treat them as unseemly. Even more essential than those professional organizational PACs is M-PAC that represents our health system. The meager dollars it raises for regional political candidates gives the UM a seat at the table where political sausage is made. Yet from that seat, our voice is disproportionally stronger than our dollars. This is because of our intrinsic legitimacy (after all, the University of Michigan is not simply a self-interested business; as a university it is one of the few institutions that are specifically here for the tomorrow of our species). The purpose of education and research is to create a better tomorrow. The obvious legitimacy of our enterprise magnifies the effect of our lobbying. My friend Rick Bossard, a critical link between the University of Michigan Health System and the world of politics and policy, once quoted a prominent state of Michigan official as saying: “Show me all the data you want, but the only thing a politician understands is a story.” So please make 2014 a year to tell those stories. A few dollars from each faculty member will make a difference. (This plug and my plug for your support of the Micah and Noah Canvasser Mott Library are all I’ll ask of you this year in terms of external philanthropy).
- Last month I complained, quixotically, that technology and health care policy have gone beyond enabling to distorting the practice of medicine. I have no illusion that technology and standardization are essential in health care, but their applications are best carefully integrated into the next iteration of our model of health care, rather than legislated by Congress, regulated by disconnected agencies and states, or put in play by competing industries in the free market. It is an unsightly hodgepodge that is forcing the commoditization of medical practice, with a misguided belief that technology will solve the problems. Health care is becoming more expensive and less patient-centric in spite of the Orwellian rhetoric that puts this phrase in play. When this gargantuan apparatus eventually collapses, correction will be all the more difficult.
- Orwellian language brings to mind ICD-10, another story of our time. Few can doubt that to manage the complexities of modern diagnoses and new therapies, some consistency in language is necessary at national and an international level. That consistency has been achieved and regulated, but now to a fault. A Darwinian niche was filled in 1893 when Jacques Bertillon, a French physician, presented the Bertillon Classification of Causes of Death at a meeting of statisticians in Chicago. Five years later the American Public Health Association recommended adopting this system throughout North America, with periodic revisions to reflect new discoveries. The idea was embraced and in 1900 it became the International Classification of Causes of Death published as a small book. In 1948 the World Health Organization (WHO) took over the responsibility for this publication, expanding it to two volumes and including morbidity conditions, injuries, their causes, and mental conditions. That sixth revision (ICD-6) in 1949 was retitled – International Statistical Classification of Diseases, Injuries and Causes of Death (ICD). A ninth revision began at an international conference in 1975 and the International Classification of Diseases, Clinical Modification (ICD-9-CM with additional morbidity data) is used by the U.S. National Center for Health Statistics (NCHS) in assigning diagnostic and procedure codes for inpatient, outpatient, and physician office utilization throughout the United States. It was updated annually.
 Work on ICD -10 began in 1983 and is only now in the midst of implementation. This “new” system became ridiculously complex in its 3 decades of creation. It is a main reason we must abandon our beloved homegrown electronic medical record called CareWeb in favor of a clunky nationally-mandated product. (See the article in New York Times Business Day by Pollack December 30, 2013: “Who knows the code for injury by Orca?” Also, Utter et al in JACS 217:516, 2013: Challenges & opportunities with ICD-10-CM/PCS). The US ICD-10 CM has 68,000 codes. That is a lot of separate diagnoses to keep straight. Amazingly, a newer system ICD -11 is expected 2015 from the WHO. With up to 16,000 diagnostic codes ICD-10 is already in play world-wide from China to the United Arab Emirates. Hearing a rumor that the code had “7 different categories for bird bites” I went to ICD10Data.com and found even more detail than I’d expected. Does this matter? I think so, for when a practitioner or office has to spend more time documenting a service (writing the note and looking up the codes for evaluation and management billing, etc.) than actually delivering the service, something is wrong. The infrastructure of personnel to manage this work in doctors offices, insurance offices, and government offices also siphon off huge dollars from actual delivery of care. Then too, if the documentation is inaccurate the bill at best is delayed or not paid, at worst the health care provider may be accused of fraud and incur penalties.
Work on ICD -10 began in 1983 and is only now in the midst of implementation. This “new” system became ridiculously complex in its 3 decades of creation. It is a main reason we must abandon our beloved homegrown electronic medical record called CareWeb in favor of a clunky nationally-mandated product. (See the article in New York Times Business Day by Pollack December 30, 2013: “Who knows the code for injury by Orca?” Also, Utter et al in JACS 217:516, 2013: Challenges & opportunities with ICD-10-CM/PCS). The US ICD-10 CM has 68,000 codes. That is a lot of separate diagnoses to keep straight. Amazingly, a newer system ICD -11 is expected 2015 from the WHO. With up to 16,000 diagnostic codes ICD-10 is already in play world-wide from China to the United Arab Emirates. Hearing a rumor that the code had “7 different categories for bird bites” I went to ICD10Data.com and found even more detail than I’d expected. Does this matter? I think so, for when a practitioner or office has to spend more time documenting a service (writing the note and looking up the codes for evaluation and management billing, etc.) than actually delivering the service, something is wrong. The infrastructure of personnel to manage this work in doctors offices, insurance offices, and government offices also siphon off huge dollars from actual delivery of care. Then too, if the documentation is inaccurate the bill at best is delayed or not paid, at worst the health care provider may be accused of fraud and incur penalties.

The list goes on by the way to include chickens, turkeys, geese, ducks, and other birds. Holy cow – have ruminants also been considered?- Current Procedural Terminology (CPT) codes describe medical, surgical, and diagnostic services and are maintained (and copyright-protected) by the AMA CPT Editorial Panel. CPT coding is similar to that of the ICD system except that the CPT identifies services rather than diagnoses. The Centers for Medicare and Medicaid Services (CMS) established the Healthcare Common Procedure Coding System (HCPCS) in 1978 as a voluntary system, but The Health Insurance Portability and Accountability Act of 199 made CPT coding mandatory. [Title I of HIPAA protects health insurance coverage for workers and their families when they change or lose their jobs. Title II – the Administrative Simplification (AS) provisions – requires the national standards for electronic health care transactions and national identifiers for providers, health insurance plans, and employers.] The U.S. ICD -10 PCS has 76,000 codes for procedures. Human disease and its therapeutic options are complex, but does a diagnostic billing system for doctors offices and hospitals need that degree of detail? Who would have thought the elements of medical practice would be so complex?
 Jumping from the complex elements of modern American healthcare structures to the relative simplicity of the truly elemental elements we come to Jöns Jacob Berzelius, (1779 -1848), a curious Swedish physician. His interests in chemistry dominated his career to the extent that he became one of the founders of modern chemistry along with Boyle, Dalton, and Lavoisier. Berzelius developed the concept of electrochemical dualism, created our system of chemical formula notation (e.g. H2O), and he originated terms including catalysis, polymer, protein, and isomer. You can thank him for the distinction between chemistry and organic chemistry. He identified or isolated a number of elements including silicon, selenium, cerium, and thorium. Students in his lab discovered lithium and vanadium.
Jumping from the complex elements of modern American healthcare structures to the relative simplicity of the truly elemental elements we come to Jöns Jacob Berzelius, (1779 -1848), a curious Swedish physician. His interests in chemistry dominated his career to the extent that he became one of the founders of modern chemistry along with Boyle, Dalton, and Lavoisier. Berzelius developed the concept of electrochemical dualism, created our system of chemical formula notation (e.g. H2O), and he originated terms including catalysis, polymer, protein, and isomer. You can thank him for the distinction between chemistry and organic chemistry. He identified or isolated a number of elements including silicon, selenium, cerium, and thorium. Students in his lab discovered lithium and vanadium.-
 Thorium, a naturally occurring radioactive element (Th -90) was discovered in 1828 by Norwegian priest and mineralogist Hans Morten Thrane Esmark, but isolated and identified that year by Berzelius. Thorium is quite relevant to us. It has the atomic number 90 and is naturally radioactive (thorium-232). It is 3-4 times more abundant on earth than uranium in the Earth’s crust and is mainly refined from monazite sands. It has been considered as a nuclear fuel and India is leading in the pursuit of that application. It is used in high-end optics and scientific instruments. Thorium produces the radioactive gas radon-220 and its other secondary decay products include radium and actinium. The radiogenic heat of the earth largely comes from radioactive decay of thorium and uranium. Thorium was named for the Norse mythologic god, Thor – associated with thunder, lightning, protection of mankind, fertility, and healing. Clearly Thor’s persona encompasses some urologic undertone. The day of the week Thursday also derives from Thor. By the way, twenty years ago yesterday (February 6, 1994) the cartoonist Jack Kirby passed away at age 76 in Thousand Oaks, California. He was the imaginative “penciller” who drew Thor for Marvel Comics.
Thorium, a naturally occurring radioactive element (Th -90) was discovered in 1828 by Norwegian priest and mineralogist Hans Morten Thrane Esmark, but isolated and identified that year by Berzelius. Thorium is quite relevant to us. It has the atomic number 90 and is naturally radioactive (thorium-232). It is 3-4 times more abundant on earth than uranium in the Earth’s crust and is mainly refined from monazite sands. It has been considered as a nuclear fuel and India is leading in the pursuit of that application. It is used in high-end optics and scientific instruments. Thorium produces the radioactive gas radon-220 and its other secondary decay products include radium and actinium. The radiogenic heat of the earth largely comes from radioactive decay of thorium and uranium. Thorium was named for the Norse mythologic god, Thor – associated with thunder, lightning, protection of mankind, fertility, and healing. Clearly Thor’s persona encompasses some urologic undertone. The day of the week Thursday also derives from Thor. By the way, twenty years ago yesterday (February 6, 1994) the cartoonist Jack Kirby passed away at age 76 in Thousand Oaks, California. He was the imaginative “penciller” who drew Thor for Marvel Comics.

-
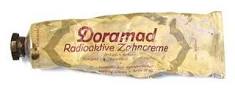 The Auergesellschaft Company of Berlin in the 1920s had the novel idea of using thorium to make radioactive toothpaste advertised to “strengthen defenses” of teeth and gums (Doramad Radioaktive Zahncreme). A related healthcare novelty, Radithor, was a patent medicine manufactured from 1918 to 1928 by Bailey Radium Laboratories, Inc., of East Orange, New Jersey. The owner of the company and head of the laboratories William J. A. Bailey, a Harvard College dropout, advertised it as “”Perpetual sunshine and a cure for the living dead.” It didn’t contain thorium, but consisted of triple distilled water with 1 microcurie of radium 226 and 228 isotopes. The Vita Radium Suppositories, also including radium and sold around 1930 by Home Health Products of Denver were advertised for “weak discouraged men.” Radium Springs, Georgia is one of the state’s “Seven Natural Wonders.” After it was found to have trace elements of radium, it became a popular therapeutic spa. Radium Springs, New Mexico also sits at the location of an old hot springs, although it never enjoyed national popularity as a resort. And then we must consider Radium Schokolade.Not all change and new technology has genuinely advanced the human condition.
The Auergesellschaft Company of Berlin in the 1920s had the novel idea of using thorium to make radioactive toothpaste advertised to “strengthen defenses” of teeth and gums (Doramad Radioaktive Zahncreme). A related healthcare novelty, Radithor, was a patent medicine manufactured from 1918 to 1928 by Bailey Radium Laboratories, Inc., of East Orange, New Jersey. The owner of the company and head of the laboratories William J. A. Bailey, a Harvard College dropout, advertised it as “”Perpetual sunshine and a cure for the living dead.” It didn’t contain thorium, but consisted of triple distilled water with 1 microcurie of radium 226 and 228 isotopes. The Vita Radium Suppositories, also including radium and sold around 1930 by Home Health Products of Denver were advertised for “weak discouraged men.” Radium Springs, Georgia is one of the state’s “Seven Natural Wonders.” After it was found to have trace elements of radium, it became a popular therapeutic spa. Radium Springs, New Mexico also sits at the location of an old hot springs, although it never enjoyed national popularity as a resort. And then we must consider Radium Schokolade.Not all change and new technology has genuinely advanced the human condition.


- If the winter doldrums are starting to get to you and you are starting to feel weak and discouraged, however, be cautious before reaching for that Doramad toothpaste to put a sparkle in your smile or those reinvigorating Vita Radium Suppositories to give you a literal kick in the butt. Novelty is important for us in that it challenges and entertains, but on the grand scale of social policy novelty should be embraced most cautiously. While ICD-10, HIPAA, the HITECH Act derived from compulsions to innovate, and while they may not be radioactive, I don’t think they have added to the greater good or happiness of mankind (except for a few very successful vendors). Enough said by me for now about ICD-10 and CPT coding, a “Thor subject” indeed.
Best wishes, and thanks for spending time on “Matula Thoughts.”
David Bloom




























