Matula Thoughts June 5, 2015
(2686 words)
Summertime, wolverines, universities & other disparate thoughts from a clinical department of medicine at the University of Michigan
1.  June at last. Even though clinical medicine is a 24/7 business, in contrast to the seasonality of the university calendar, we can’t help but notice that summer has arrived. Ann Arbor is a glorious place to be this time of year when you can walk along, fish, kayak, or canoe the Huron River (shown above with the Gandy Dancer in the distant background). Our applicants for residency training from the west coast or south see none of this lovely environment when we interview them in late November, a real recruiting disadvantage. Nevertheless, we have again recruited a superb resident and fellow cohort to start training with us next month. Spring and summer also bring the pleasure of seeing and hearing the birds in our neighborhoods. Surviving another rough winter and hatching their 2015 chicks, they bring to mind John James Audubon, who, born 230 years ago (April 26, 1785) in Haiti, documented and detailed all sorts of American wildlife, birds especially. His Birds of America is thought to have been the first book acquired by the University of Michigan after it moved to Ann Arbor in 1837. I learned this in an article by Kevin Graffagnino in The Quarto, the quarterly publication of our Clements Library [Fall-Winter 2014]. Kevin is the Director of the Clements, one of the crown jewels of the UM. The library’s magnificent reading room with its periodic displays is an ennobling place to spend a little time, although you will have to wait until the current renovations are completed.
June at last. Even though clinical medicine is a 24/7 business, in contrast to the seasonality of the university calendar, we can’t help but notice that summer has arrived. Ann Arbor is a glorious place to be this time of year when you can walk along, fish, kayak, or canoe the Huron River (shown above with the Gandy Dancer in the distant background). Our applicants for residency training from the west coast or south see none of this lovely environment when we interview them in late November, a real recruiting disadvantage. Nevertheless, we have again recruited a superb resident and fellow cohort to start training with us next month. Spring and summer also bring the pleasure of seeing and hearing the birds in our neighborhoods. Surviving another rough winter and hatching their 2015 chicks, they bring to mind John James Audubon, who, born 230 years ago (April 26, 1785) in Haiti, documented and detailed all sorts of American wildlife, birds especially. His Birds of America is thought to have been the first book acquired by the University of Michigan after it moved to Ann Arbor in 1837. I learned this in an article by Kevin Graffagnino in The Quarto, the quarterly publication of our Clements Library [Fall-Winter 2014]. Kevin is the Director of the Clements, one of the crown jewels of the UM. The library’s magnificent reading room with its periodic displays is an ennobling place to spend a little time, although you will have to wait until the current renovations are completed.
[White House copy of 1826 painting of Audubon Portrait by John Syme]
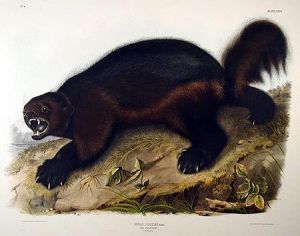
2. Gulo gulo. While Audubon is best known for his birds, his work also extended to mammals and included the Viviparous Quadrupeds of North America, produced in 1845-48. The Quarto, mentioned above, included an image of a wolverine from the Quadrupeds (shown below). A miniscule number of wolverines still exist in the lower 48 states, but their Darwinian niche is contracting and it is unlikely that you or I will ever see one in the wild. Of note, a wolverine was spotted in Utah at a nocturnal baited camera station last summer. Kevin’s article says: “By one account, Ohioans were responsible for pinning the name ‘wolverine’ on Michiganians, claiming that they shared the animal’s ill temper and greedy nature.” Buckeyes can be relied upon for charming perspectives of their northern neighbors.
The wolverine (Gulo gulo) is the largest land-dwelling species of the weasel family (Mustelidae). They have weights generally of 20-55 pounds but males have been found as large as 71 pounds. Their fur is thick and oily, making it very hydrophobic and resistant to frost. Like other mustelids their anal scent glands are very pungent. Aggressive hunters and voracious eaters, wolverines are extremely rare in Michigan outside of the Big House. The skull and teeth are the most robust of carnivores their size, allowing them to eat frozen meat and crush large bones. Gulo comes from the Latin term for glutton.
[National Park Service photo in Wikipedia. Taken in 1968]
[Wikipedia Commons, author Zefram, 2006]
[Wolverine ranges – Wikipedia]
3. Linnaeus, nomenclature and humanity’s obesity. The identification of the wolverine as Gulo gulo is a convention of biologists that traces back to Carl Linnaeus in the 18th century (1707-1778). This Swedish physician got his professional start with a medical practice that rested heavily on its urological aspects and provided him the opportunity to initiate an academic career in Uppsala at the university where he developed his enduring nomenclature system. His university remains one of great institutions of worldwide academia.
Returning briefly to Gulo gulo, Linnaeaus never anticipated modern molecular biology, but ironically GULO also turns out to be L-gulonolactone oxidase, an enzyme that makes the precursor to Vitamin C in most living creatures although not Homo sapiens. GULO is nonfunctional in Haplorhini (namely us dry-nosed primates) as well as some bats, some birds, and guinea pigs. Loss of GULO activity in primates occurred around 63 million years ago when they (we) split into wet-nosed and dry-nosed suborders (Strepsirrhini and Haplorhini). It has been speculated that the critical mutation leading to loss of GULO production benefited survival of early primates by increasing their uric acid levels and enhancing fructose effects leading to fat accumulation and weight gain. (Johnson et al. Trans. Am Clin Climatol Assoc. 121:295, 2010) The human susceptibility to scurvy thus is a likely side effect of one of the critical evolutionary steps in the making of modern man. This amazing thought leads back to the University of Michigan and our beloved colleague Jim Neel, the founding chair, in 1956, of our Department of Human Genetics, that I believe was the first in North America, if not the world. Towards the end of his life, Jim often showed up for lunch in our medical center’s cafeteria, always toting his old well-traveled knapsack, and we had a number of provocative conversations on such matters as the biology of morality. Johnson refers specifically to Jim’s landmark “thrifty gene” paper of 1962 [Am J Hum Genetics. 1962;14:353-62] wherein Neel suggested that genetic adaptation of our primate ancestors to famine may have left modern day humans with an increased risk for obesity and diabetes when foods became plentiful. Johnson notes that while the thrifty gene hypothesis was initially well received “the inability to identify the specific genes potentially driving this response has reduced enthusiasm for the hypothesis.” Johnson’s 2010 paper revisits Neel’s hypothesis and argues that at least 2 critical mutations led to our genetic adaptation to famine: the silencing of genes necessary for Vitamin C synthesis and for uric acid degradation. These two “knock-outs” enhance the effect of fructose in increasing fat stores.
4. Universities. The durability of Linnaeus’s university is no fluke. Darwinian forces have kept universities in play since their origin in the Middle Ages, and since then even grown their relative effect in society. When you think about it, it seems that universities are the only truly durable organizations that are legitimately here “for tomorrow.” A modern academic, David Damrosch, demonstrated this durability by quoting a study from the Carnegie Council, so permit me to repeat his observation. “A report by the Carnegie Council in 1980 began by asking how many Western institutions have shown real staying power across time. Beginning with 1530, the date of the founding of the Lutheran Church, the authors asked how many institutions that existed then can still be found now. The authors identified sixty-six in all: the Catholic Church, the Lutheran Church, the parliaments of Iceland and of the Isle of Man – and sixty-two universities.” [Damrosch D. We Scholars. Changing the Culture of the University. Harvard University Press. 1996. p. 18] This is a powerful observation. For all their annoying features (medieval hierarchy, guild mentality, ecclesiastical titles, indentured work force, elitism, resistance to change, decentralization) universities function primarily to educate the next generation and advance knowledge.
5. Named lectures. William J. Mayo, a graduate of the University of Michigan Medical School in 1883, left us $2000 as “a perpetual endowment for a yearly Mayo Lecture on some subject connected with surgery.” So that the fund could grow, he gave the first two lectures himself (1924 and 1925) and had his younger brother Charlie (a graduate of Northwestern University’s medical school in 1887) give the third lecture. Except for 1929, 1930, and 1945 the tradition has been continued. Reed Nesbit was the speaker in 1968. This year our colleague and friend Skip Campbell gave a superb talk called “From volume to value: charting a course for surgery.” He discussed our incipient brave new era wherein payments to health systems and individual physicians for services will disconnect from clinical volume alone (which is easily measured and indisputable) to parameters of quality and value (which are not so indisputably measured).
[Skip Campbell]
6. Dick and Norma Sarns, friends and neighbors, have impacted our world and local community beyond easy measure. The impact of their company in Ann Arbor, Sarns Inc., innovator and producer of heart lung machine technology, has been incredible. The Sarns device was the one used by Dr. Christian Barnard in 1967 for the first human heart transplant. Other Sarns devices followed and the company was acquired in time by 3M and is now owned by Terumo Corporation. Cardiac rehabilitation became the next focus of Dick and Norma with their next company, NuStep, Inc. As benefactors to our community through the Ann Arbor Area Community Foundation, the University of Michigan, and numerous other nonprofits, the Sarns family has been uncommonly generous with astute focus on building a better tomorrow. The Sarns story is now permanently embedded in the larger University of Michigan narrative in the Sarns Professorship in Cardiac Surgery. The choice of Rich Prager as the inaugural Sarns Professor is fitting. You may recall that Rich gave a magnificent Chang Lecture on Art and Medicine for us in 2013. You can revisit the talk in his subsequent JAMA article on the murals of Henry Bethune (JAMA: PN Malani, RL Prager, “Journey in Thick Wood: The Childhood of Henry Norman Bethune”, JAMA, October 8, 2014, Volume 312.) Endowments such as the Sarns Professorship will allow the University of Michigan Medical School and Health System to recruit and retain the best of the best in academic medicine to teach the next generation, to discover new knowledge and technology for tomorrow, and to do these in the milieu of our essential deliverable – kind and excellent patient care.
[Top: Dick & Norma Sarns. Bottom: Richard Prager]
[Standing ovation for Rich Prager]
7. Next week we will recirculate 3 three existing urology professorships in a ceremony that is long overdue (June 10 at 4 PM in the BSRB Auditorium). The Valassis endowment, originally given to Jim Montie by George Valassis, has grown enough to be split into two independent professorships. Ganesh Palapattu will be installed as the George and Sandra Valassis Professor, previously held by David Wood. Khaled Hafez will receive the George Valassis Professorship, previously held by Jim Montie. Julian Wan has taken over the Nesbit Professorship, occupied up till recently by Ed McGuire. These professorships will continue in perpetuity. These conjoined celebrations of the past and investments in the future will exist as long as the University of Michigan stands. We will need more endowed professorships here in Ann Arbor if we are to remain at the top of the game as a leader and one of the best in academic medicine as federal and clinical funding of medical education and research continue to slip.
8. The American Urological Association met in New Orleans this mid-May, having last convened in the Crescent City in 1997. University of Michigan faculty and residents had well over 100 abstracts, posters, podium sessions, and panels in addition to dozens of committee meetings. While it is impossible to even mention but a fraction of these, the MUSIC collaborative initiated by Jim Montie, deployed so excellently by David Miller and now assisted so well by Khurshid Ghani, was a highlight. This collaborative has brought many urologic practices and other urology centers outside the UM to podiums at the AUA in the interest of improving urologic care and practice. The quality, value, and safety of health care cannot effectively be managed centrally by government, industry, or national organizations such as the American Board of Medical Specialties. These attributes of excellence must be played out at the bedsides, clinics, operating tables, hospitals and in the offices of committed practitioners. Lean process believers would say that improvements in complex systems are most efficiently and effectively recognized and tested in the workplace, at the “Gemba” (lean process engineering terminology for workplace). Just as central management of a nation’s economy failed in the Soviet Union, central regulation of quality, safety, and “value” is a doomed experiment. Collaboratives such as MUSIC, built on trust and a desire to improve patient care, work best at the local and regional levels. An educational and social reception at the AUA showcased MUSIC and David Miller challenged the group to extend its work beyond prostate cancer to other urologic conditions. Walking through the main hallway of the giant convention center at the AUA meeting I kept seeing Toby Chai and Ganesh Palapattu on the video screen in the Rising Stars display. Michigan had a heavy presence at the AUA again this year.
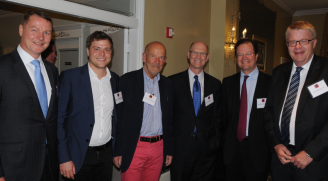
9. Our Nesbit Reception hosted more than 130 alumni, friends, faculty, and residents. For me the Nesbit Society events are high points of the year. We held this event at the 100 year-old Le Pavilion Hotel. Although hit hard by Katrina in 2005, Le Pavilion took in many of its employees with their families and pets in the wake of the devastation, yet was back up and running as a hotel by December of that year. The social part of a profession, especially a profession as social as medicine, is an essential part of its substance and pleasure and the Nesbit Society serves this function well. We had a large contingent from Denmark and the University of Copenhagen including Jens Sönksen and his daughter Louise who was a little girl when they lived in Ann Arbor. Barry Kogan, Bart & Amy Grossman, Marty & Anne Sanda, Kathleen Kieran, and our contributions to the Northwestern urology program (JO DeLancey, Diana Bowen, & Drew Flum) were on hand. So too were Sarah Fraumann and Jackie Milose who will both be doing reconstructive urology for the University of Chicago but at polar ends of the city. Stephanie Kielb of course is in the middle of the city on the Northwestern faculty. Jill Macoska was back from Boston and Bunmi (E. Oluwabunmi Olapade-Olaopa) was the most distant traveler, hailing from Ibadan, Nigeria. Many other former students and friends joined our faculty and residents for a lovely evening that Mike Kozminski and Julian Wan put together with Sandy Heskett and April Malis. Our next Nesbit event will be in the autumn (October 15-17), deep in the midst of football season and we have great expectations for our pigskin wolverines. With a new coaching staff on the scene we can well understand the need to have put aside our annual prostate cancer fund raiser, the Michigan Men’s Football Experience. It must be “first things first” for Coach Harbaugh’s team this inaugural year. While fund raisers come and go, our work in the Medical School and Health System remains nonstop without seasonality. Urologic research at Michigan continues to progress, with a number of exciting findings and technologies in play that will be discussed in upcoming departmental What’s New communications.
[Above-Danish contingent: L-> R Stefan Howart from Coloplast, Peter Oestergren, Lasse Fahrenkrug, Eric Halvarsen, André Germaine, Jens Sönksen. Bottom: Jens & Louise]
[Top-Barry Kogan Chair at Albany, Bart Grossman from MD Anderson; Bottom-Lindsey Herrel, Cheryl Lee, & Marty Sanda Chair at Emory]
[Top–Takahiro Osawa, Noburo Shinohara, Takahiro Mitsui; Bottom-Lindsey Cox, Yahir Santiago-Lastra, Anne Cameron]
[Alon Weizer, Jackie Milose, Mary Nowlin, Liz Marsh]
[Bunmi Olapade-Olaopa, Peter Knapp, Quentin Clemens]
10. It is worth reflecting upon telltale signals that we either pick up or miss. On this particular day in 1981 the Morbidity and Mortality Weekly Report of the Centers for Disease Control and Prevention reported that five people in Los Angeles, California, had a rare form of pneumonia seen only in patients with weakened immune systems. At the time this observation was a matter of only faint curiosity to most physicians, and of even less interest to the public at large until it turned out, in retrospect, to have been the first recognized cases of AIDS. In the crowded bandwidth of everyday clinical life, narrow subspecialty focus, and the administrative hassles of the practice of medicine it is important to keep a deliberate open mental channel tuned to the greater environment of healthcare and science. Many telltale signs that presage tomorrow surround us and one wonders what telltale signals we are missing amidst today’s noise and summertime moments.
Upcoming events: Residents graduation dinner. Triple professorship installation. Chang Lecture on Art and Medicine Thursday July 16 – Dr. Pierre Mouriquand Professor Claude-Bernard University, Lyon, France: “Slowly down the Rhône: the river and its artists.”
Thanks for spending time on “Matula Thoughts” this month.
David A. Bloom